From the epicenter of the nation’s COVID-19 impacts in New York City to a neonatal unit in Minneapolis, Minnesota, Gustavus Adolphus College alumni are on the front lines in responding to the coronavirus pandemic in a healthcare setting.
We asked two doctors and two nurses to reflect on the past three months, how their work has changed, and where they find hope. These young alumni are optimistic, steadfast, and grateful for their supportive communities—but don’t take it from us.
Here they are, in their own words…
Ben Biewen ’13, MD
Emergency Medicine Resident
Bellevue Hospital/NYU Langone | Manhattan, New York City

I majored in biology at Gustavus and went to the Creighton School of Medicine in Omaha after graduation. I originally planned to work in pediatrics, but I fell in love with emergency medicine during a clinical rotation in my third year of medical school. After moving to New York City last June, I’ve been doing month-long rotations in different emergency units at Bellevue and NYU.
I was in the pediatric emergency unit when we started hearing about coronavirus in January, then I rotated into the ICU right when things were ramping up in New York City. Pretty quickly, our work became strictly taking care of COVID-19 patients in negative pressure rooms or suspected cases who were waiting for test results. The number of medical teams assigned to the ICU tripled and most of the patients on my floor were on ventilators. Hardly any visitors were allowed, so I ended every shift by calling the patients’ families to give them nightly updates.
Now I’m in the emergency room, seeing patients right when they arrive at the hospital. My head’s still down, just working day to day to do whatever I can to provide the best possible care for my patients, but it’s been amazing to see the outpouring of support—food donations from restaurants, entire neighborhoods cheering every night at 7 p.m. It’s been a crazy couple of months, but COVID-19 numbers are starting to slow here a little bit. Throughout this situation, our goal has been to provide exceptional care to our patients while also taking care of one another as healthcare providers.
It’s a hard time right now, but this is why I picked emergency medicine. You never know what’s going to walk through the door or how old the person is or what issues might exist. I like that we’re always going, always asked to use high-acuity problem solving. Anytime someone comes to the emergency room, they’re scared. Being the first person the patient sees is an opportunity to care for them by being knowledgeable and comforting in a difficult time.
This is what I chose to do.
Emee Udo ’18, RN
Neonatal Intensive Care Nurse
Children’s Minnesota Hospital | Minneapolis, Minn.

The Gustavus nursing program prepared me for the world of medicine. And when it comes to crisis, I think Gustavus taught me a lot. First and foremost that crisis is defined differently by everyone and that everyone responds differently. I think I gained a worldly view through my professors and my classes to the point where I am able to put my privilege aside and see this situation through the lens of those being much more heavily impacted.
During COVID-19, a normal shift starts with arriving on time as opposed to 20 minutes early to avoid unnecessary congregating in the break room. When I get to the unit, I check my assignment and am handed a surgical mask. My tasks at work haven’t changed much—we are still caring for babies, working in close contact with parents in order to do two-person cares and assist with kangaroo care among other things. Our visitors are now limited to two caregivers for the duration of the patient’s stay. For some babies, that’s a week, but for most of our patients that’s multiple months or even a year. That’s the hardest change, seeing excited grandparents meet their grandbaby over FaceTime and not being there for them as they are sometimes fighting for their lives.
The most special thing I’ve seen was one of our long-term patients getting to Skype her parents as she opened her Easter basket. Technology has been amazing in helping us bridge the gap during this difficult time. We have also received numerous meals, baked goods, t-shirts, homemade masks, thermometer donations, and words of encouragement from individuals and organizations which have meant the world to me and my coworkers. We work with a special population that has yet to be severely impacted by this virus, so it’s easy for us to overlook ourselves as ‘frontline’ during this time and it’s especially impactful when someone goes out of their way to thank us.
What helps me through challenging times? Knowing that I get to wake up and go to work and do my dream job. I have job security. I am healthy. I am able to move my body each day. I feel safe at home. I have the financial resources to buy food to sustain myself. I have the technology needed to stay connected with loved ones. That is more than a lot of people can say right now, and not a day goes by that I don’t feel immense gratitude for my situation.
Brian Berglund ’09, MD
Chief Resident, Internal Medicine
Abbott Northwestern Hospital | Minneapolis, Minn.
During my time at Gustavus, I earned extra money working as a school bus driver in Saint Peter. I wanted to find a career like that—something based on human connections and serving people. I went to medical school because I was fascinated by human physiology and inspired by professors like Margaret Bloch Qazi and Michael Ferragamo.
Right now, the hospital is an entirely different place than it was in February. Nearly no visitors are allowed in the hospital, only staff and patients. Everyone is wearing masks at all times, and the hospital is only half-full—we’ve cleared as much room as we can in anticipation of a surge in COVID-19 cases. COVID-19 patients present to the hospital with a varying range of symptoms and severity of illness, and we have to wear full personal protective equipment (PPE) when treating them. Outside of treatment for patients, I’ve been spending most of my time working on practices to keep our healthcare providers and other staff safe. Lots of video meetings, reviewing scheduling guidelines, communicating policy changes, and supporting our resident physicians.
Patients are scared and providers are rapidly learning more about this novel virus and the illness it manifests. COVID-19 can cause a significant pneumonia and breathing difficulties, even for young people who are healthy otherwise. The silver lining to all of this is seeing people come together to fight a common enemy. I think the nurses, respiratory specialists, medical assistants, phlebotomists, and technicians are especially inspiring. They’re fearless and committed, and they’re the ones who are largely responsible for building that sense of community.
It’s been really rewarding to set up face-to-face video conferencing for patients to be able to see and speak to their family members. Some of them haven’t seen their loved ones for weeks. It’s special to be at their bedside and see that moment of connection. It’s also been powerful to see patients come off ventilators. Everybody cheers.
The rigor of academics at Gustavus require you to be steadfast and thoughtful. That’s been helpful in piecing together the things required to understand and treat this illness. Today, my work takes place in a team within the infrastructure of a hospital. A hospital is its own community, just like campus is. Being a Gustavus student and football player gave me a foundation for what it means to be a good teammate and a good community member.
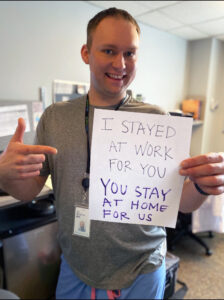
We’re all in this together now, all working towards a common goal. If you can, please stay at home. This isn’t just about doctors and nurses—everyone has to come together to make this work.
We are all a community, and we all rely on each other.
Stephanie Hardel Krautkremer ’11, RN
Cardiac/Surgical Intensive Care Nurse
North Memorial Health Hospital | Robbinsdale, Minn.

I was a biology major and neuroscience minor at Gustavus and attended grad school at the University of Minnesota to earn my master of nursing degree. I am now employed at North Memorial Hospital in Robbinsdale, where I am a nurse on the cardiac/surgical intensive care unit, which has turned into a COVID-19 ICU.
The last month has been extremely interesting. We have cut all elective procedures, so our overall numbers at the hospital have been extremely low. For my unit, things are beginning to pick up. We were very slow a few weeks ago. Now we are completely full of patients that are waiting to hear back on their COVID-19 test results or patients that are positive. A ‘normal day’ consists of getting to work, finding my brown paper bag that contains my mask and face shield that we have to reuse, getting my assignment, and starting my care. When it comes time to leave, I am super cautious about what I bring in my house—I usually leave anything work-related in the garage and throw my scrubs in the washer immediately!
To slow the spread of the virus, we have not let visitors into the hospital. I think my biggest moment of clarity about how awful this pandemic has become came when I first had to call a family member to let them know their loved one was being intubated because of increasing respiratory needs. For me, that’s one of the hardest aspects of right now…trying to explain to family what is going on without them being able to witness it for themselves.
All of the nurses, physicians, and staff have been really great about helping and supporting each other during this time. I like to think that building close-knit relationships at work, like the ones I built at Gustavus, has helped prepare me for this crisis. Now, more than ever, we have leaned on each other. Knowing that we, as nurses, are helping fight a global pandemic is pretty motivating. Some of the patients on my unit are extremely ill, and being able to care for them and cheer on small victories in their progress back to health is enough to keep me coming back every day.